SALEM ALATON
Special to the Globe and Mail, Toronto
If you’ve still got the teeth for it, you may owe your dental hygienist a big smile.
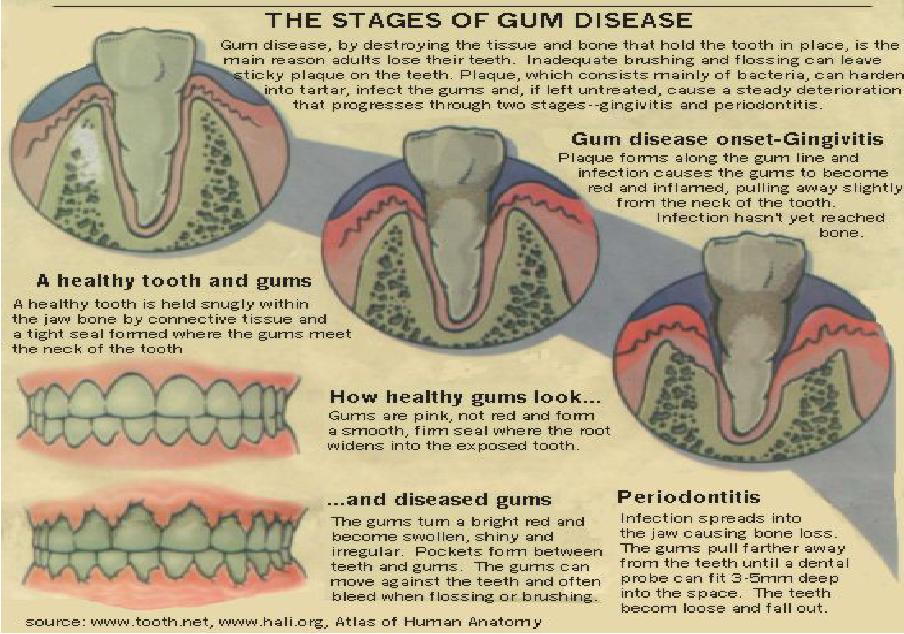
Gingivitis and periodontitis – inflammation and disease of the gums have long been the oral hygiene problems that led to the loss of teeth in the elderly. Baby boomers, still scoffing at admonitions about regular brushing and flossing, are now getting to the age where they find themselves in trouble. “Periodontal disease is a disease,” declares Audrey Newcombe, instructor in the dental assistants’ program at Holland College in Charlottetown, PEI and past president of the Canadian Dental Hygienists Association.” People don’t think of it that way but it is. It can be very invasive and very unnoticeable at the same time.”
The problems, from the swollen, tender gums of gingivitis to the increasing destruction of soft tissue and ultimately bone in periodontitis, “happen so gradually that people thought that was the way it was supposed to be,” Ms. Newcombe adds. Studies have found that about half of older adults have some degree of gingivitis; up to 20 per cent of the entire population have some degree of periodontal disease.
But dentists say it need not be for the vast majority of people, including most elderly, if they put consistent effort into oral hygiene. Daily brushing and flossing routinely break down the natural and continuous build-up of bacteria in the mouth, the waste products of which form a substance called Plaque As plaque accumulates around the teeth, gum tissue responds with an inflammation reaction called gingivitis.
“You get shiny gums that look like bruise fruit, ” observes Ginny Cathcart, co-ordinator of the dental-hygiene program at Vancouver Community College. “You touch them and you’ll get pink blood on the toothbrush.” This plaque-associated gingivitis is the most common form of the condition, although there are other categories, including gingivitis brought on by pregnancy (steroid hormone influenced gingivitis) HIV-associated gingivitis and gingival enlargement prompted by certain medications.
“Not everybody that gets gingivitis will eventually get periodontal disease,” says Ms. Cathcart, “but everybody that has periodontitis had gingivitis to start with. It’s important to treat gingivitis.” Ms. Cathcart says a high-fibre diet will stimulate the gums and vitamin C will aid good blood flow. But prevention and treatment of gingivitis should centre on bathroom ablutions and periodic professional care. Brushing should be done with a softbristled brush, gently but persistently penetrating along the gumline and do it for several minutes rather than 30 seconds. Electric toothbrushes, once a laughable piece of ‘1960’s kitsch, are now much refined and are sometimes recommended by dentists for their ability to follow the contours of the gums.
Flossing, a routine followed daily by as few as 15 per cent of adults, penetrateg the tighter crevices between teeth that the brush can’t reach, disrupting bacteria colonies where it passes. And on a visit to the dentist’s office, manual scaling and planing with sharp instruments removes the plaque which has hardened into tartar, also known as calculus.
With brushing and flossing, “it’s the thoroughness of the job rather than how you do it,” James Brookfield, a past president of the Canadian Dental Association whose practice is in Kirkland Lake, Ont. Daily rinsing with an antiseptic mouthwash is also a useful part of the regimen, adds Dr. Brookfield, an adviser to the Listerine Oral Health Information Bureau in Toronto. (Prescription mouthwashes are sometimes advised by dentists for gingivitis.) Periodontitis, often the result of gingivitis that has gotten out of control, occurs when the gum tissue adhering to the tooth starts to degenerate and reveals what is called attachment loss.
WHAT CAUSES BAD BREATH?
Bad breath or halitosis has a range of causes extending from renal failure to sinus infections and blocked salivary glands. One of the potentially useful things about halitosis, in fact, is that it can signal a condition that requires treatment, including gingivitis, periodontitis and other dental problems such as untreated cavities and abscess.
“There are 360 [types of] bacteria that populate the oral cavity,” explains Ginny Cathcart, co-ordinator of the dental hygiene program at Vancouver Community College. “In an unhealthy situation, there are 10-to-20 types that take hold.”
Halitosis-generating bacteria in the teeth are the kind that can flourish with very little oxygen, breeding unrestrictedly in dark, inaccessible crevices. Brushing, flossing, rinsing with antiseptic mouthwash and periodic dental appointments will all discourage these promiscuous opportunists.
– Salem Alaton
“The tooth is sitting with the gum around it like a turtleneck sweater,” explains Dr. Brookfield. “If you can insert a probe into there about two to three millimetres it may be all right, but if you can go in five or six millimetres, then it goes too far.”
When the destruction of periodontitis extends from the soft tissue of the gums to the bone of the jaw, the teeth themselves are in danger of being lost. There may be a degree of genetic suscetibility to periodontitis, and conditions like diabetes and various immune disorders can significantly exacerbate the tendency. Smoking, as usual, heads the list of avoidable risks.
“Tar and nicotine are very destructive to oral tissue,” says Ms. Newcombe. “People who are smokers really are heading down a path of periodontal disease almost inevitably.” Treatment for periodontal disease starts with scaling and root planing, traditionally with the dentist getting inside the gumline at the tooth wall with a metal instrument (curette) and scraping away the calculus. Today, “we rely more on ultrasonic instrumentation for this, which allows you to remove the tartar or calculus much more effectively,” comments Howard Tenenbaum, head of periodontics at the University of Toronto faculty of dentistry. He likens this hard tartar to a coral reef.
If problems persist, deeper scaling and planning is attempted. A majority of patients respond well to these initial procedures. Beyond this, antibiotics can come into play, testing having been done during the scaling to identify the specific bacteria that are dominant in the disease. A new generation of antibiotics can be applied topically, inserted into specific places in the gums where attachment loss is creating an urgent problem. “Periodontitis is a chronic disease and it can recur,” notes Dr. Tenenbaum, who is also director of periodontics at Mount Sinai Hospital in Toronto. “That’s where topical antibiotics can be useful, when people have two or three spots that are acting up.”
When the disease is too advanced however, with pockets of loose gum tissue so deep that other methods cannot help, periodontal surgery “is still one of the mainstays of treatment,” Dr. Tenenbaum says.
The standard gingivectomy to remove degenerated gum tissue has evolved now to include procedures that make a flap of the gum, allowing greater access to the tooth’s roots for further cleaning and with healing and cosmetic advantages.
Like the gingivitis that precedes it, periodontitis comes in various forms, including rare juvenile and prepubertal types that afflict youngsters. Commonplace adult periodontitis is a potential issue for people from their twenties on, but the upside is that risks needn’t escalate sharply with advancing years. The principle reason the elderly are more prone to gum disease, as periodontal experts such as U of T’s Dr. Richard Ellen have argued, is that their capacity to maintain oral hygiene diminishes.
About 85 per cent of patients being treated for periodontal disease have the problem halted, Dr. Tenenbaum says. For those with refractive or treatment- resistant disease, “now we’re on the cusp of developing regenerative treatments, which is very exciting,” he remarks.
While bone grafts have to date been only moderately successful, a process called 11 guided tissue regeneration” using a synthetic membrane has potential, as do the use of new biological materials such as bone and enamel proteins.
A Severe/Refractory Periodontal Disease and Investigative Unit at U of T is also exploring such questions as genetic susceptiblity and the potential benefits of anti-inflammatory agents and osteoporosis drugs for treating gum disease.
For the vast majority of Canadians, however, warding off periodontitis comes down to what they do to prevent or treat those swollen gums which Dr. Tenenbaum calls “the battlefield between the microbes and the body.”
